mms
MMS eliminates even the most resistant bacteria - study
Elimination of antibiotic-resistant bacteria with chlorine dioxide
How Chlorine Dioxide destroys - eliminates, even the most antibiotic-resistant bacteria. Study.
Chlorine Dioxide MMS - Miraculous Mineral Solution, eliminates bacteria that are resistant to antibiotics. Scientific research - study.
SUMMARY
Bacterial antibiotic resistance (AMR) is a problem in all regions, with six pathogens accounting for 73.4% of deaths due to bacterial AMR, namely Escherichia coli (E. coli), Staphylococcus aureus (S. aureus), Klebsiella pneumoniae (K. pneumoniae), Streptococcus pneumoniae (S. pneumoniae), Acinetobacter baumannii (A baumannii) and Psuedomonas aeruginosa (P. aeruginosa).
The World Health Organization launched a Global Action Plan for AMR in 2021, which is still active - the healthcare costs for AMR amount to several billion dollars worldwide.
A review on antimicrobial resistance commissioned by the UK government claimed that AMR could kill 10 million people a year by 2050 and has emerged as one of the biggest public health threats of the 21st century.
Only one AMR pathogen, methicillin-resistant Staphylococcus aureus (MRSA), caused more than 100,000 deaths worldwide, while the other four pathogens covered in this study still cause as many deaths.
The present research focused on studying the efficacy of chlorine dioxide in eliminating five different AMR bacteria in vitro as a novel and effective treatment.
This study used different concentrations of chlorine dioxide with five antibiotic-resistant bacteria, ranging from 1 - 7 ppm concentrations. The disinfection studies were compared to controls and the results showed greater than 95% disinfection with 7 ppm concentrations.
Chlorine dioxide is a size-selective antimicrobial agent that can quickly kill micrometer-sized organisms, but will not cause real harm to much larger organisms, such as animals or humans, as it cannot penetrate deeply into their living tissues.
It is safe when used in low concentrations for short durations. Clinical trials should be conducted to gain experience in the best doses and protocols for eliminating antibiotic-resistant microorganisms from the body.
Download the study here:
ERADICATION OF ANTIBIOTIC RESISTANT BACTERIA USING CHLORINE DIOXIDE (335 downloads )
Introduction
The five antibiotic-resistant bacteria we incorporated into this research study included Escherichia coli ( Escherichia coli ), methicillin-resistant Staphylococcus aureus ( Grape Sickness ), Klebsiella pneumonia ( Pneumonia Clebsiella ), Acinetobacter baumannii ( Acinetobacter acinetobacter ) and Pseudomonas aeruginosa ( Pseudomonas aeruginosa ).
The World Bank Group in 20171 warned that in 2050, drug-resistant infections could cause global economic damage compared to the 2008 financial crisis.
AMR also threatens the achievement of several of the UN's sustainable development goals, in particular the goals for good health and well-being.
Hospital costs were estimated at over €900 million in 2007.3 Outpatient costs were €10 million and labour productivity losses were €150 million.
In addition, the loss of productivity due to mortality from infections was estimated at around €450 million per year. This economic cost would be significantly higher using the figures reported in the Global Burden of bacterial antimicrobial resistance in the 2019 report.
Given the widespread spread of AMR bacteria worldwide and the fact that antibiotics are becoming less and less effective, finding other more natural and innovative ways to eradicate these killers is essential.
WHAT IS CHLORINE DIOXIDE - LIVE VIDEO FOR CRITICS.
Chlorine dioxide is a safe and effective way to eliminate these AMR bacteria without creating further resistance. The discovery of new natural antibacterial agents with novel mechanisms of action remains a high priority globally.
Post-treatment of antibiotic-resistant bacteria More than 150 antibiotics have been developed since the discovery of penicillin in 1940 and for most available antibiotics resistance has occurred in the bacteria being treated.
Based on this, by 2050, the number of deaths could be staggering - one person every three seconds.
Bacteria have resisted almost every antibiotic developed in the last 50 years.
There is a positive correlation between antibiotic use and prevalence, with higher rates in countries with higher use.
Inappropriate prescribing by doctors who wrongly prescribe antibiotics for other infections, such as viral or fungal infections, instead of bacterial infections.
There is a hypothesis that overuse of antibiotics is associated with inappropriate prescribing and administration of antibiotic therapy.
Irresponsible use of antibiotics is the main problem of antibiotic resistance. The influence of antibiotics is now waning due to the progressive increase in resistance seen in all antimicrobial drugs.
Increased antibiotic resistance is due to a combination of microbes exposed to antibiotics and the spread of these microbes and their resistance mechanisms.
Not only do antibiotics become less effective, but their use can also cause dysbiosis, especially in the gut or sites of secondary infections.
The impact on human health can be devastating: over-use of antibiotics has been shown to destroy most of the natural gut flora.
Pharmaceutical companies are also reluctant to invest in antibiotic development for a number of reasons, including low market returns, restrictions on antibiotic use, scientific difficulties in developing antibiotics and the current regulatory environment.
The route to finding new antibiotics and developing them into medicines is long and expensive.
It costs $800 million to $1 billion to bring a new drug to market - on average, it takes more than ten years to enter the clinic.
Due to the time pressure we face in the battle against AMR, a different approach is needed to explore alternatives to antibiotic therapy.
Compared with all underlying causes of death in the Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) 2019, antimicrobial resistance (AMR) would be the third leading cause of GBD level 3 deaths in 2019, based on the counterfactual of no infection - only ischaemic heart disease and stroke accounted for more deaths that year.
In addition, many hospital pathogens may not be eliminated by routine cleaning; thus, they can survive for long periods of time in hospitals, indoor air and surfaces and contribute to the transmission of infections.
Alternative therapies are a promising field of research. It is therefore imperative to pursue new, innovative treatments for AMR, and this is the foundation of this research - the use of natural substances to eradicate AMR, such as MRSA, E coli, S aureus, K pneumoniae, A baumannii and P aeruginosa, that do not build up further resistance.
The discovery of new natural antibacterial agents with novel mechanisms of action remains a high global priority.
Natural antimicrobials have been successfully used to treat bacteria12 and have been the main source of medicines throughout human existence, which is important to remember.
Natural products, including medicinal plants, remain widely popular today, with around 80% of the world's population relying on herbal products and related supplements as part of their treatment regimen.
Natural products such as Rosmarinus officinalis12 and Mangifera indica L., Anacardiaceae, 14 antimicrobial peptides, plant essential oils and their combinations have been shown to be quite effective in inhibiting a wide selection of bacterial pathogens, including the five AMR bacteria in the present study.
This study examines the elimination of antibiotic-resistant MRSA, Escherichia coli, Klebsiella pneumonia, Acinetobacter baumannii and Pseudomonas aeruginosa with CDSpure ampoules containing 2,990 ppm per 5 ml ampoule of 16 chlorine dioxide in vitro.
Importance of the five antimicrobial-resistant bacteria Acinetobacter baumannii Acinetobacter baumannii includes Gram-negative, strictly aerobic, non-fermentative, non-gastrointestinal, non-motile, catalase-positive and oxidase-negative bacteria.
Although A. Baumannii represents a relatively low proportion of total bacteremia cases, multidrug resistance is globally problematic for this species.
Globally, over 71% are multi-drug resistant.
In the United States, 27% of patients with mechanical ventilation were colonized with a multi-resistant strain of A. baumannii.
A. baumannii uses resistance strategies including chromosomal β-lactamases, efflux pumps and aminoglycoside modifying enzymes.
Following exposure to human serum albumin, A. baumannii upregulates the transcription of β-lactamases, indicating potential intrinsic mechanisms of antimicrobial resistance in serum.
Due to the prevalence of infections and outbreaks caused by multidrug-resistant A. baumannii, few antibiotics are effective for treating conditions caused by this pathogen.
Several reports have shown that A. baumannii rapidly develops antimicrobial resistance and multiresistant strains have been isolated.
The World Health Organization (WHO) has also identified A. baumannii as a critical priority pathogen that poses a significant threat to human health and for which new antibiotics are urgently needed.
Escherichia coli E. coli is often resistant to multiple classes of antimicrobials among the strains that cause urinary tract infections and bacteremia exceeding 50%.
E. coli is a versatile Gram-negative bacterium, easily found and susceptible to natural and random genetic changes.
It is 1-3 x 0.4-0.7 µm in size and 0.6-0.7 µm in volume.
Klebsiella pneumoniae ( Klebsiella pneumoniae )
Klebsiella pneumoniae strains are usually classified as opportunistic, hyper-resistant (hyKp) or multidrug-resistant (MDR).
While classical K. pneumoniae (cKp) consists of opportunistic strains that are often associated with hospital-acquired infections, superbug strains are considered community bacteria that can infect people of all ages, including healthy individuals.
The rapid spread of multi-resistant K. pneumoniae strains is a major threat to global health, as these strains are responsible for many hospital-acquired infections with high morbidity and mortality.
Clebsiella pneumoniae is described as a Gram-negative, encapsulated and non-motile bacterium.
Methicillin-resistant Staphylococcus aureus (MRSA) MRSA is considered one of the most dangerous hospital pathogens causing many difficult-to-treat infections in hospitals and was named hospital-associated MRSA (HA-MRSA).
Over the last 20-25 years, MRSA has been isolated from community environments, giving rise to Community Associated MRSA (CA MRSA).
MRSA can cause various organ infections, most commonly skin and subcutaneous tissues, followed by invasive infections such as osteomyelitis, meningitis, pneumonia, pulmonary abscess and emphysema.
Infectious endocarditis caused by MRSA is associated with increased morbidity and mortality compared to other organisms and is associated with intravenous drug abuse.
Methicillin-resistant Staphylococcus aureus (MRSA) is a Gram-positive cocci that is both catalase- and coagulase-resistant.
Pseudomonas aeruginosa (Ψευδομονάδα αεριογόνος)
The Ψευδομονάδα αεριογόνος is among the top five causes of hospital-acquired bacteremia, often leading to sepsis.
P. aeruginosa is an important Gram-negative opportunistic pathogen that causes many serious acute and chronic infections with high morbidity and mortality of up to 40%.
What makes P. aeruginosa a particularly challenging pathogen is its high intrinsic and acquired resistance to many of the available antibiotics.
It is an opportunistic human pathogen capable of causing many life-threatening acute and chronic infections, especially in patients with compromised immune defences. It is of particular importance as it is the leading cause of morbidity and mortality in patients with cystic fibrosis (CF).
Chlorine dioxide (ClO2) Antimicrobial Chlorine dioxide (ClO2) is a yellow to reddish-yellow gas that can decompose rapidly in air.
Chlorine dioxide has a molecular weight of 67.452 g/mol and a solubility in water at sea level of 3.01 g/L (3000 ppm) at 25 °C and 34.5 mm Hg.
It is an effective biocide at concentrations as low as 0.1 ppm and over a wide pH range. Even in cold water, it is ten times more soluble than chlorine.
The chlorine dioxide has a lower oxidation potential than ozone and chlorine.
The optimum pH is between pH 6.0 and pH 10.0 and is generally more effective against microorganisms at pH above 8.0 than chlorine.
When it reacts in water, it forms chlorite ions, a very active chemical that can kill bacteria and microorganisms in any solution.
The chlorine dioxide quickly kills bacteria, viruses and Giardia and is effective against cryptosporidium.
Chlorine dioxide also improves taste and odour, destroys sulphides and phenols, controls algae and neutralises iron and manganese ions.
It is an effective biocide at concentrations as low as 0.1 ppm and over a wide pH range.
Chlorine dioxide, biofilm and resistance.
Chlorine dioxide is more suitable for therapeutic use, as it can penetrate and eliminate biofilm.
According to Simpson et al. (1993)54 , chlorine dioxide can remove biomaterials quickly because it is highly soluble in water.
Unlike ozone, it does not react with the extracellular polysaccharides in the biofilm.In this way, chlorine dioxide can quickly penetrate the biofilms to reach and kill the microbes living inside the film.
Penetration of biofilms to eliminate microorganisms is a real challenge for both natural and allopathic medicine.
Biofilm is a three-dimensional structure formed by microbial cells that adhere to biotic or abiotic surfaces under various physiological and environmental factors that have yet to be determined.
In addition, these cells constantly multiply and produce extracellular polymeric substances (EPS), forming a matrix that surrounds these microbes.
Biomaterials are aggregates of microbial cells surrounded by self-producing matrices of exopolysaccharides on biotic or abiotic surfaces.
Biofilms show significant protection against antibiotics, host immune defences and adverse environmental conditions compared to free cells.
It is estimated that 65-80% of human infections are caused by biofilm-forming bacteria.
Biofilms are estimated to be 1000 times more resistant to antibiotics than free cells.
The interaction between bacterial cells and environmental factors triggers biofilm formation.
Chlorine dioxide can penetrate and eliminate biofilms, a major advantage over many antibiotics that cannot do this.
Another very important advantage of the therapeutic use of chlorine dioxide over antibiotics is that it cannot create bacterial resistance to antibiotics.
The presence of the four amino acids (cysteine, methionine, tyrosine and tryptophan) and in particular cysteine and biological thiols play a crucial role in all living systems, including microbes, so that no microbe can develop resistance to chlorine dioxide.
Chlorine dioxide penetrates bacterial cell walls and reacts with vital amino acids in the cell's cytoplasm to kill the organism.
The by-product of this reaction is chlorite, which is not known to pose significant risks to the environment or human health.
Safety and effectiveness of chlorine dioxide
In 1967, the US EPA first registered the liquid form of chlorine dioxide for use as a disinfectant and sanitizer.
Chlorine dioxide is a size-selective antimicrobial agent that can rapidly kill micron-sized organisms, but cannot harm much larger organisms such as animals or humans, as it cannot penetrate deep into their living tissues.
Chlorine dioxide cannot penetrate deep into the tissues of larger organisms and the circulation of larger organisms provides a constant supply of antioxidants, offering protection from the effects of chlorine dioxide oxidants.
Other research has shown that chlorine dioxide, a powerful oxidant, can inhibit or destroy microorganisms at concentrations ranging from 1 to 100 ppm, producing potent antiviral activity, inactivating > or equal to 99.9% of viruses within 15 seconds for sensitization.
Georgiou (2021) successfully demonstrated the efficacy of chlorine dioxide against MRSA in-vitro, with 99.99% - 100% growth inhibition even at low concentrations.
Ongoing research at the Innerlight Biological Research Foundation has been investigating the clinical use of chlorine dioxide, including non-specific spores, bacteria and viruses, for many applications for over twenty-five years.
Extensive clinical applications of chlorine dioxide in Epstein-Barr virus (EBV), cytomegalovirus (CMV), hepatitis A, B virus, HIV (AIDS virus) and others are in continuous use.
On 14 October 2020, the Bolivian parliament passed a bill (ley 1351) allowing the use of chlorine dioxide as a medicine against COVID 19.
Chlorine dioxide has been used successfully in countries such as Bolivia, Mexico, Peru, Brazil and Colombia.
In Bolivia, Law No. 1351 of 2020 was adopted (Official Gazette of Bolivia, 2020), which approved the manufacture, marketing, supply and use of chlorine dioxide solution for prevention and treatment in view of pandemic COVID 19.
More recently, in 2021, a study by Insignares Carrione conducted to determine the efficacy of orally administered chlorine dioxide in the treatment of COVID-19 showed that chlorine dioxide is effective in the treatment of COVID-19.
Chlorine dioxide has three atoms - scientists call this bond an "unstable" or "negatively charged" ion.
When this bond of atoms separates, a very small subatomic pulse of energy is created. This pulse occurs when chlorine dioxide passes around pathogenic microorganisms in the body.
It only attacks "acidic" and "anaerobic" microbes (viruses, bacteria, fungi or parasites) in the body and will not damage the microbiome.
These bacteria survive only without oxygen and include many pathogenic organisms.
Anaerobic organisms have not developed sufficient defences against the onslaught of oxygen, especially oxygen in progress, and quickly succumb to its lethal action.
All healthy cells that need oxygen to live or are "alkaline" are safe.
Toxicology of chlorine dioxide
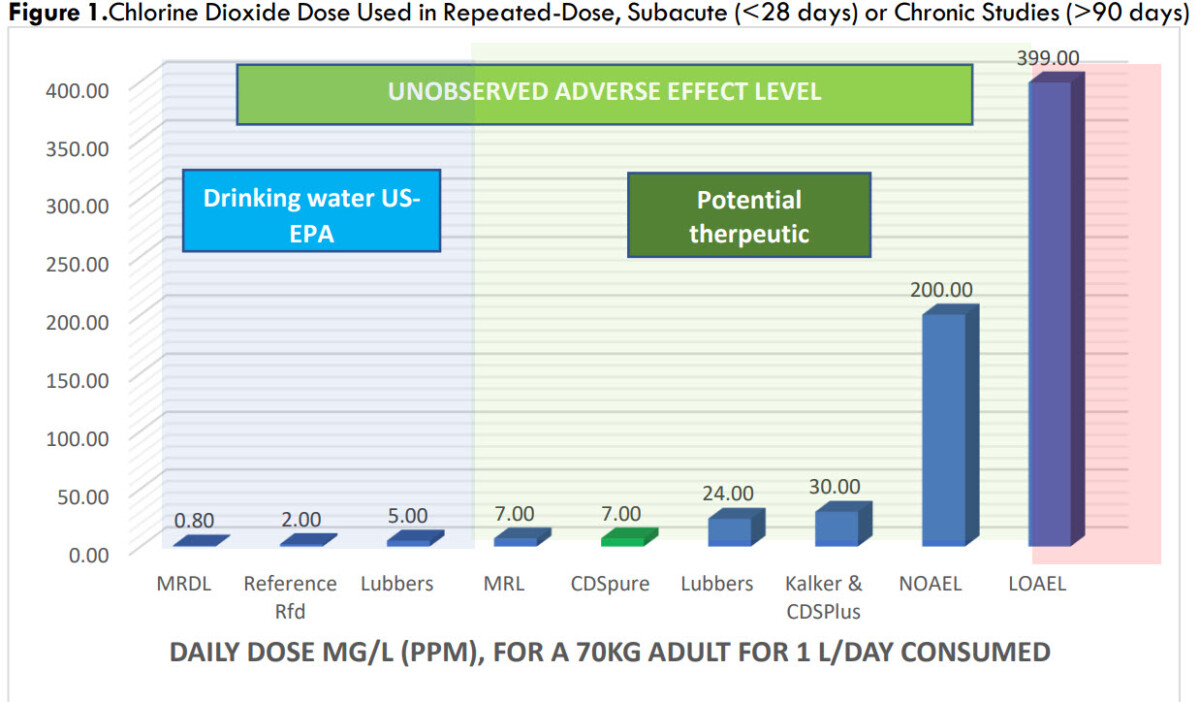
Figure 1 shows the reference levels for drinking water disinfection from the US Environmental Protection Agency (blue zone).
Levels of potential therapeutic efficacy in experimental animals with zero toxicity are shown in the green zone. Toxic levels are shown in the red band (above 399 ppm).
The 5 ppm level that eliminated 99% or more antibiotic-resistant bacteria in this study is within the blue/green zone of zero toxicity.
Figure 1. Dose of chlorine dioxide used in repeated dose, subacute (90 days) studies
Chlorine dioxide is added to drinking water to protect people from harmful bacteria and other microorganisms.
Most people are exposed to small amounts of chlorine dioxide and chlorite by drinking treated water, including food, as it is used as a disinfectant in the food industry.
There is no evidence that chlorine dioxide or chlorite affects reproduction in humans.
Reproduction studies in male animals do not consistently demonstrate alterations in spermatogenic markers, abnormal morphology or motility; however, the reported effects occur at doses higher than the adverse developmental effects.
Similarly, changes in haematological parameters occur at higher doses. No information on death in humans following oral exposure to chlorine dioxide was identified.
In a study by Scatina, 70 human volunteers drank chlorine dioxide in solution up to 24 ppm and experienced no adverse effects.
Methodology Materials and methods
Five antibiotic-resistant bacteria were used in the present study; E coli, S aureus, K pneumoniae, S pneumoniae, A baumannii and P aeruginosa.
All were obtained from a certified laboratory (ATTC, Germany) in a frozen vial and grown on blood agar plates.
A sample of each bacterium was taken from the isolated cultures using a sterile loop in a Class II safety cabinet from the culture plates and placed in sterile tubes containing 5 ml of soybean cryptic broth (TSB).
These culture tubes were incubated at 37 degrees Celsius in a Heraeus incubator. Once a reasonable number of tubes were reached, the tubes were frozen and then stored in liquid nitrogen at - 176 degrees Celsius until use.
Bacterial count
When quantifying bacteria in laboratories, it is common to count the number of colony-forming units, which is a simple method that gives a good overview of cell viability.
A major drawback is that it takes days to obtain results, which will vary from technology to technology based on sample preparation techniques and conditions.
In this study, bacterial counts were obtained using the QUANTOM Tx™ microbial cell counter from Logos Biosystems.
It is an automated image-based cell counter that can identify and count individual bacteria within minutes.
QUANTOM Tx automatically focuses, captures and analyses multiple fluorescently stained cell images to detect bacterial cells with high sensitivity and accuracy.
It contains a sophisticated cell detection and decompression algorithm that can accurately identify individual bacterial cells even in the tightest clusters.
In these experiments, we used the Viable Cell Staining Kit to detect live or viable cells versus dead cells.
To prepare the sample for the QUANTOM counter, 10 microlitres (µl) of culture medium was taken using a DLAB electronic pipette previously calibrated and placed in a sterile 1.5 ml Eppendorf tube.
To this was added 2 μl of Viable Cell Staining Dye, which was incubated in a Heraeus incubator at 37 degrees Celsius for 30 minutes.
To this sample 8 μl of buffer was added to enhance the fluorescent signal.
Preparation of chlorine dioxide solution
For the preparation of the chlorine dioxide solution, a 5 ml ampoule of chlorine dioxide called CDS Pure® containing exactly 2,990 ppm of chlorine dioxide (CAS 10049- 04-41) manufactured by AQARIUS pro-life was used for the experiments.
It is a ready-to-use, sterile chlorine dioxide solution in a sealed glass ampoule that is ultra-pure nanofiltered, pH-neutral and chlorine-free.
The chlorine dioxide solution (demineralised water, chlorine dioxide) does not contain residues, silver ions or nanoparticles. Since each 5 ml ampoule contains exactly 2,900 ppm of chlorine dioxide, it is easy to determine how many millilitres are required.
The concentrations used ranged between 1 - 7 ppm chlorine dioxide.
The quantities used for each concentration were 1 ppm = 1,667 µl CDS Pure®, 2 ppm = 3,344 µl, 3 ppm = 5,016 µl, 4 ppm = 6,688 µl, 5 ppm = 8,336 µl, 6 ppm = 10,032 µl and 7 ppm = 11,704 µl. The exposure time was irrelevant, as disinfection was immediate, within seconds.
Chlorine dioxide was added to these tubes at different concentrations.
The concentration of 5 ml of chlorine dioxide CDS used in the experiment ranged from 1,667 µl (1 ppm) to 11,704 µl (7 ppm), added to the tubes with a DLAB electronic pipette and gently mixed for each bacterium.
For each experimental tube, a control tube was also prepared from the same culture medium.
Depending on the amount of chlorine dioxide applied to the experimental tube, the same amount of distilled water was added to the control tube to keep the dilution factor constant.
From these control and experimental tubes, 6 μl of sample was taken using an electronic pipette and placed on the M50 cell counting slides.
The slides were placed in the QUANTOM centrifuge for 8 minutes at 300 RCF (Relative Centrifugal Force) and then placed in the QUANTOM microbial cell counter to obtain a baseline measurement (Control) and another measurement from the Experimental Tube.
The optimal settings of the QUANTOM microbial cell counter for the different bacteria were determined according to the shape and size of the different bacteria to optimize the counting.
Results
To evaluate the ability of chlorine dioxide to disinfect the five types of antibiotic-resistant bacteria in this study, 5 ml ampoules of CDSpure were used throughout, as these ampoules contain a standard concentration of 2,990 ppm.
Concentrations were from 1 ppm to 7 ppm, in 1 ppm increments. Control and experimental samples at the various concentrations were taken in triplicate, for which the average was taken for each.
These values were compared with the control sample without CDSpure chlorine dioxide.
In general, in all five bacterial studies, there was greater than 95% disinfection at the maximum concentration of 7 ppm chlorine dioxide, while some species were eliminated at lower concentrations of 4 - 7 ppm (t-test, p<0.01).
Let's look at each type of bacteria separately in the tables and figures below.
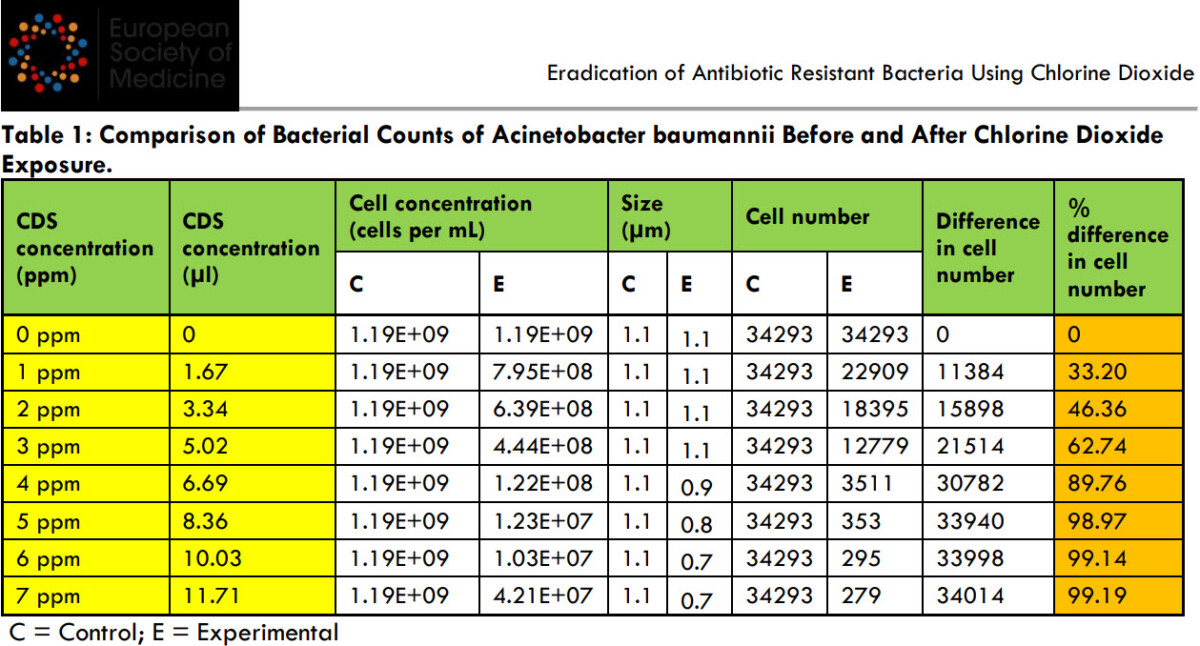
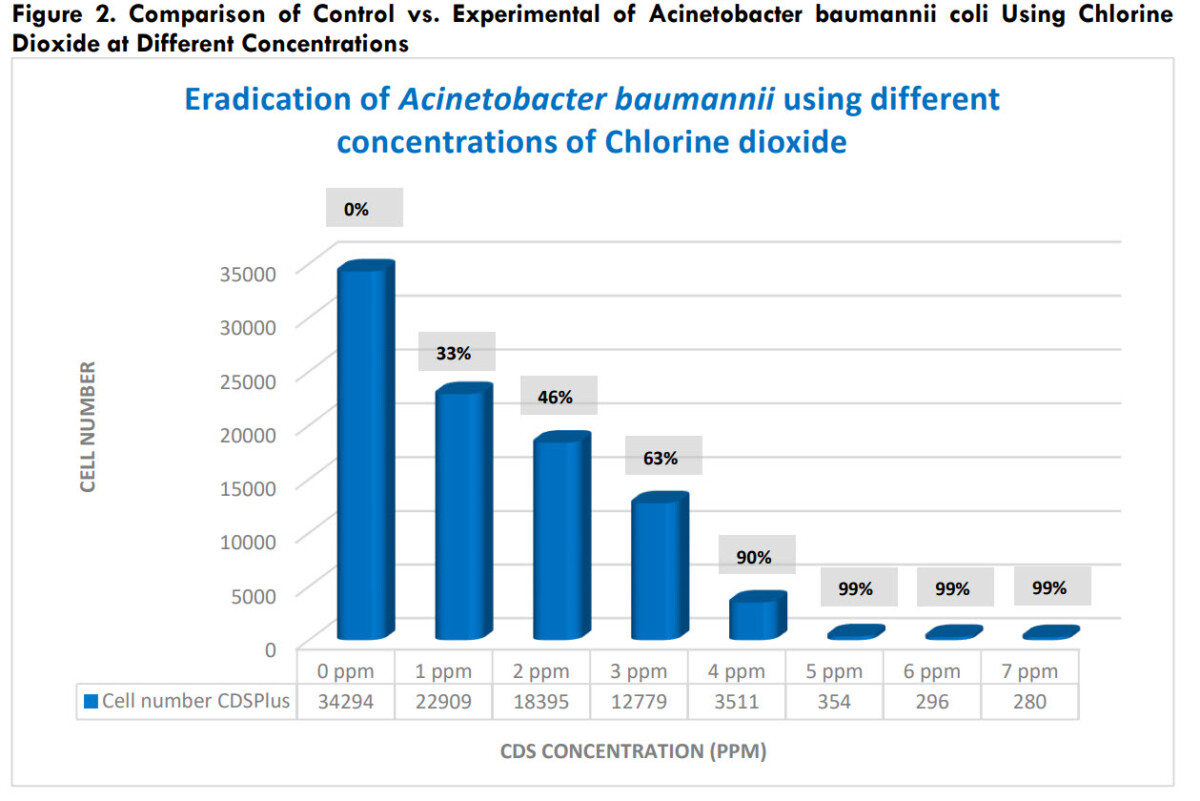
Disinfection of Acinetobacter baumannii With Acinetobacter baumannii, there was 99% disinfection at concentrations of 5, 6 and 7 ppm chlorine dioxide (t-test, p<0.01) (Table 1, Figure 2).
Comparison of bacterial counts of Acinetobacter baumannii before and after chlorine dioxide exposure
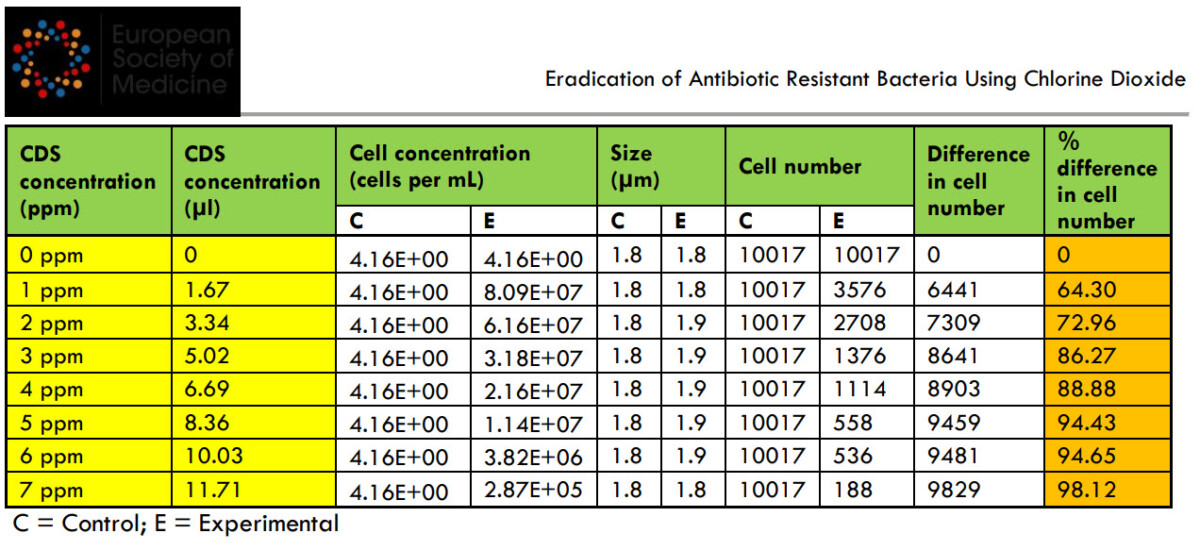
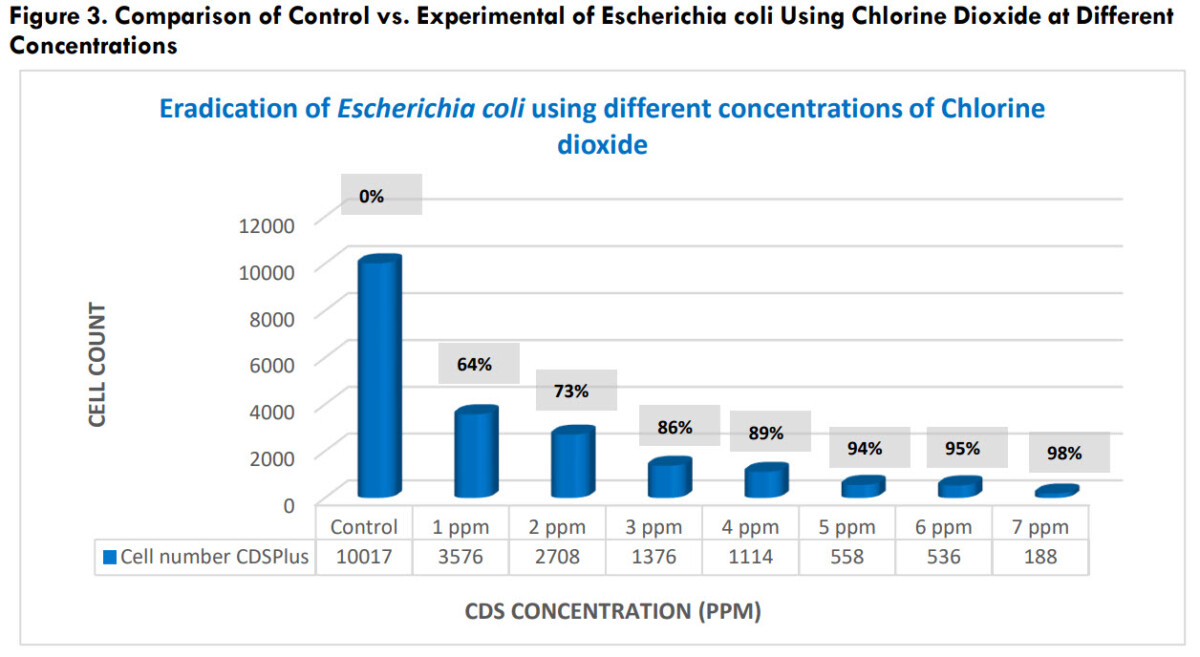
Disinfection of Escherichia coli
With E. coli, there was > 98% disinfection at a chlorine concentration of 7 ppm (t-test, p<0.01) (Table 2, Figure 3).
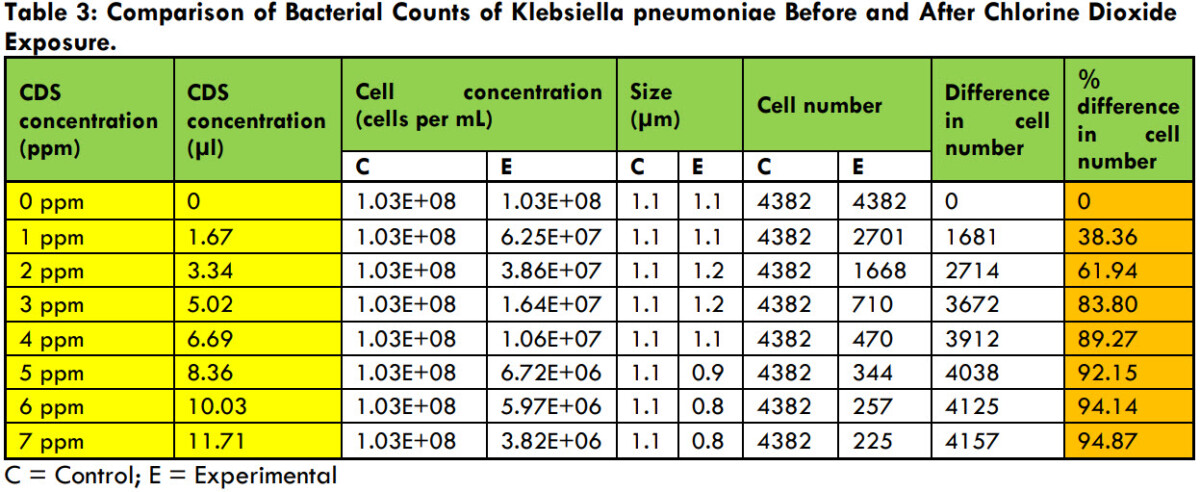
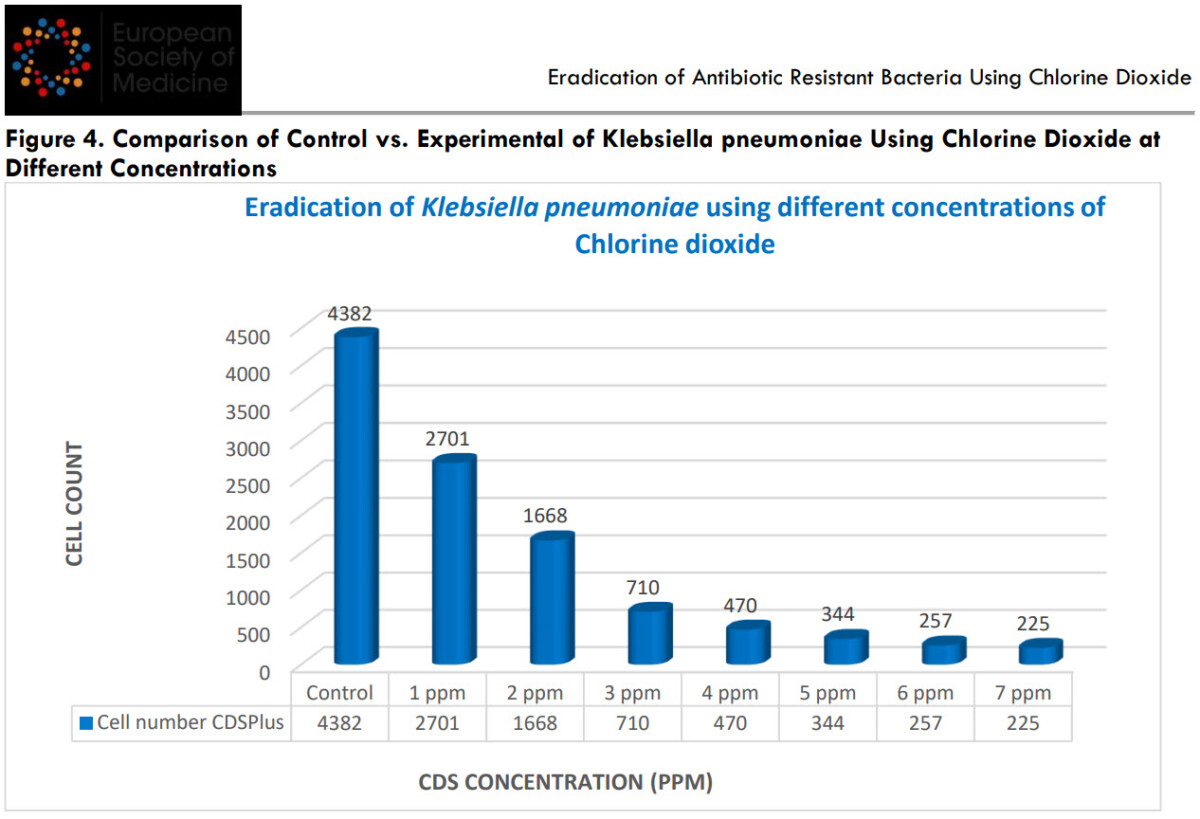
Disinfection of Klebsiella pneumoniae
With K. pneumoniae bacteria, there was > 94% disinfection at chlorine concentrations of 6 and 7 ppm (t-test, p<0.01) (Table 3, Figure 4).
Table 3: Comparison of the number of Klebsiella pneumoniae bacteria before and after chlorine dioxide
Έκθεση
Comparison of Klebsiella pneumoniae bacterial counts before and after chlorine dioxide
Comparison of control versus experimental control of Klebsiella pneumoniae using chlorine dioxide in Concentrations
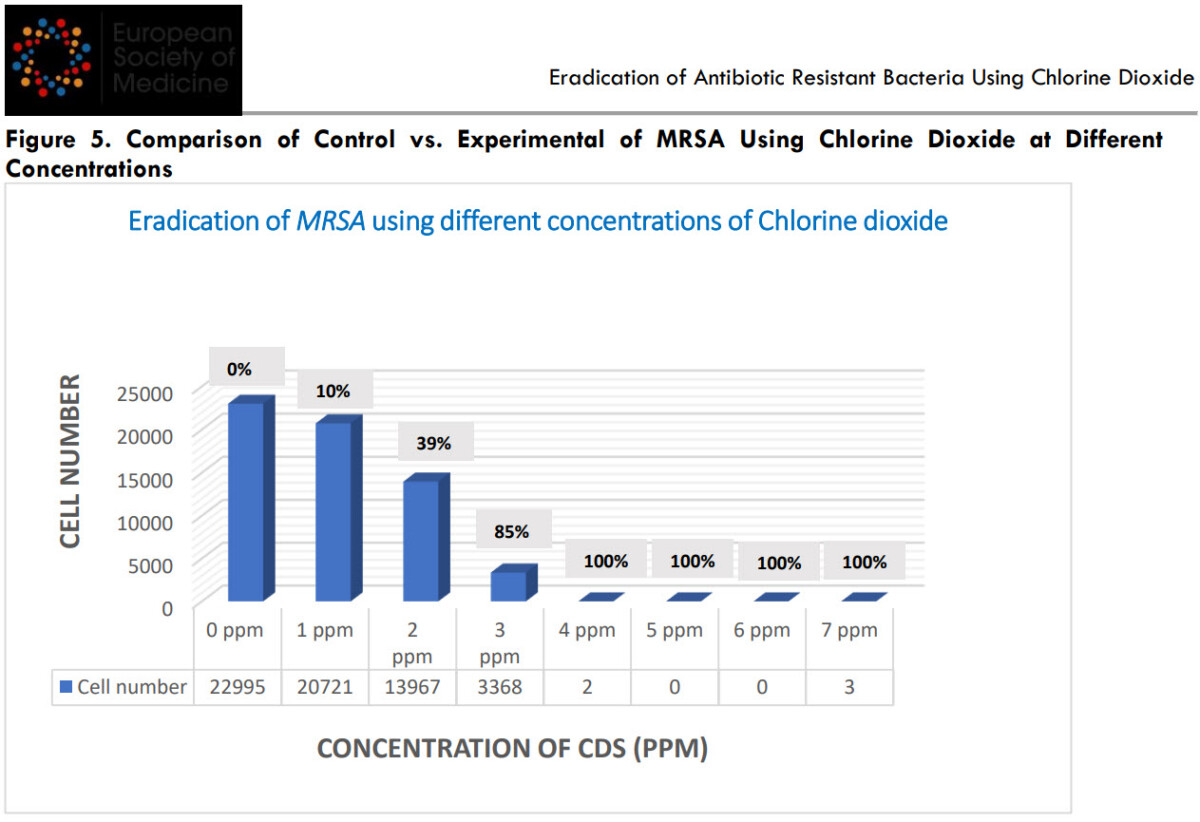
Disinfection of methicillin-resistant Staphylococcus Aureus (MRSA)
With MRSA, there was > 99% disinfection at a chlorine concentration of 4 - 7 ppm (t-test, p<0.01) (Table 4, Figure 5).
Table 4: Comparison of the number of MRSA bacteria before and after exposure to chlorine dioxide.
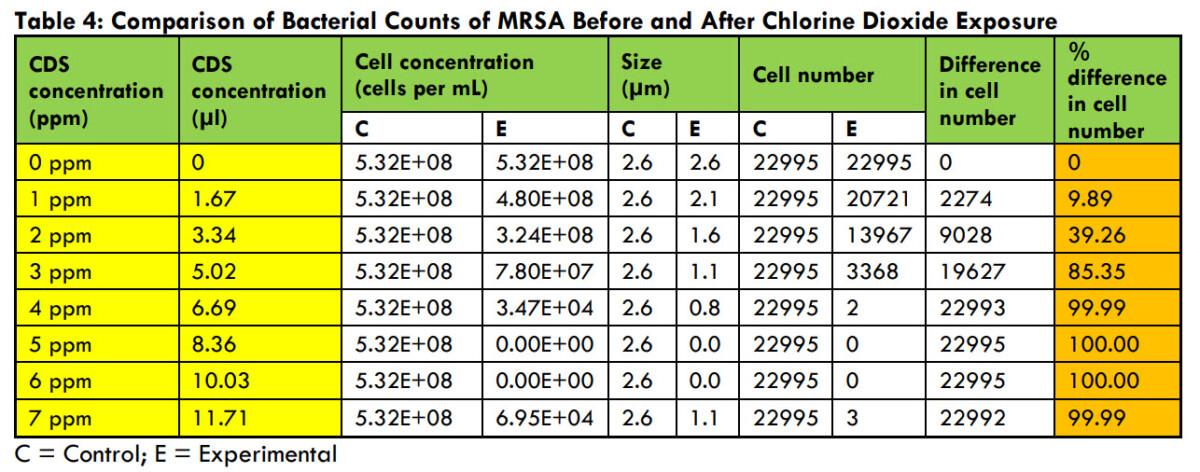
Figure 5. Comparison of control versus experimental MRSA using chlorine dioxide at different Concentrations.
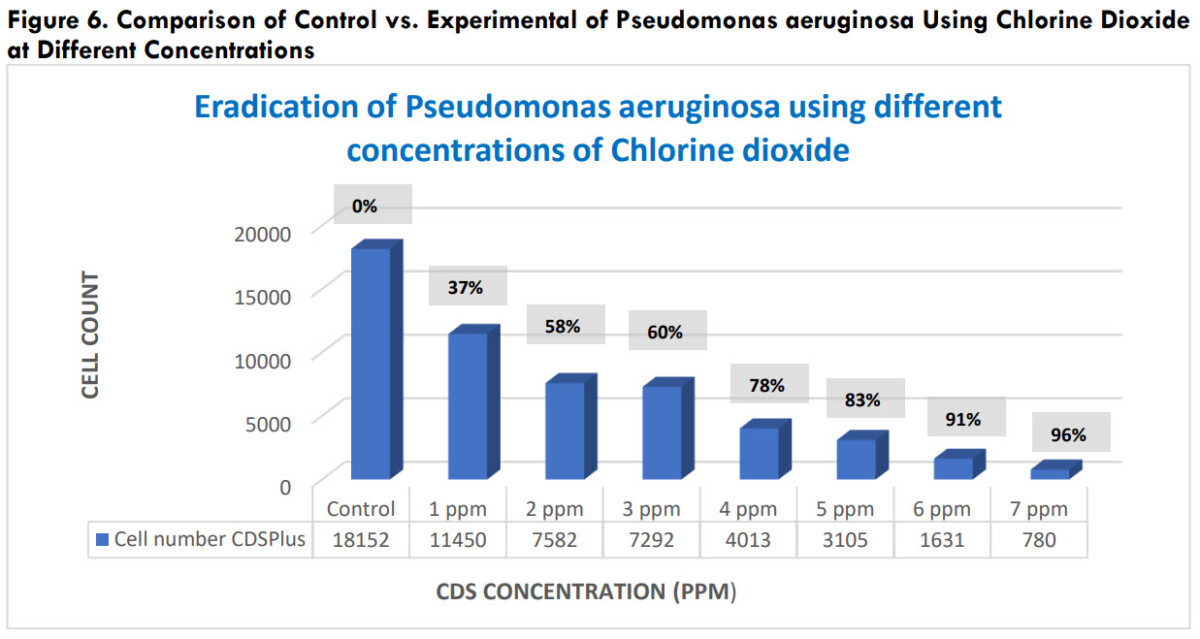
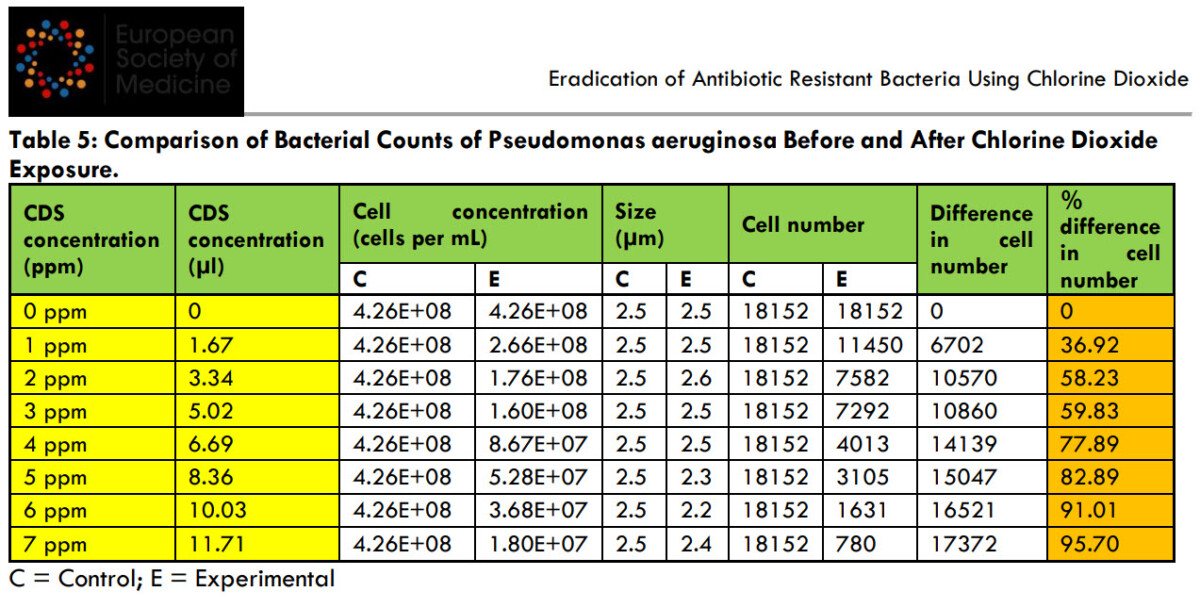
Pseudomonas aeruginosa disinfection With P. aeruginosa bacteria, there was >95% disinfection at a chlorine concentration of 7 ppm (t test, p<0.01) (Table 5, Figure 6).
This research shows that chlorine dioxide solution is an effective natural substance that can eliminate all types of antibiotic-resistant bacteria tested.
The chlorine dioxide concentrations required to achieve 95% or greater disinfection for the five antibiotic-resistant bacteria are between 4 and 7 ppm, which are within the potentially safe limits a (see Figure 1).
Σχήμα 6. Σύγκριση ελέγχου έναντι πειραματικού της Pseudomonas aeruginosa με χρήση διοξειδίου του χλωρίου σε διαφορετικές συγκεντρώσεις.
Figure 6. Comparison of control versus experimental Pseudomonas aeruginosa using chlorine dioxide σε διαφορετικές συγκεντρώσεις.
Table 5: Comparison of Pseudomonas aeruginosa bacterial counts before and after chlorine dioxide
Έκθεση.
Έκθεση.
Discussion
The rise of antibiotic-resistant bacteria is a major threat to public health worldwide. These resistant bacteria have developed resistance to conventional antibiotics, making infections increasingly difficult to treat and leading to increased mortality rates and higher healthcare costs.
Reported annual mortality is expected to exceed 10 million by 2050 from antibiotic-resistant diseases, surpassing deaths from cancer.
This poses a serious threat to global health, as infections that were once treated quickly can now lead to prolonged illness, causing great suffering and strain on the healthcare system.
Ο αντίκτυπος της έρευνας σε εναλλακτικές προσεγγίσεις για την εξάλειψη των ανθεκτικών στα αντιβιοτικά βακτηρίων δεν μπορεί να υποτιμηθεί. Η έρευνα αυτή μπορεί να σώσει ζωές σε παγκόσμια κλίμακα μέσω των εξής:
1. Improving patient outcomes: Alternative strategies can effectively treat infections that were once considered untreatable.
By successfully targeting antibiotic-resistant bacteria, these approaches can improve patient outcomes, reduce morbidity and mortality rates and restore hope to people suffering from resistant infections.
2. Reduced healthcare burden: The increasing burden of antibiotic-resistant infections is straining healthcare systems worldwide.
By finding alternative ways to combat resistance, the burden on healthcare resources can be reduced, resulting in improved efficiency, reduced hospital stays and lower healthcare costs.
3. Epidemic prevention: If left unchecked, resistant bacteria can cause widespread epidemics.
Research into alternative approaches offers the opportunity to prevent the emergence and spread of resistant strains, ultimately safeguarding public health and preventing large-scale epidemics.
4. Differentiation of treatment options.
New and natural treatments provide alternative approaches to fight antibiotic resistance.
Broaden the range of treatment options available to healthcare providers, ensuring they have multiple tools to fight resistant infections.
This differentiation increases the chances of successful therapeutic outcomes and helps to overcome the limitations of conventional antibiotics.
5. Overcoming resistance mechanisms: Antibiotic-resistant bacteria have developed sophisticated mechanisms to avoid the effects of traditional antibiotics.
New and natural therapies offer the potential to target bacteria through different pathways, bypassing or overcoming existing resistance mechanisms, providing a new approach to fighting resistant strains and reducing the likelihood of treatment failure.
6. Reduced side effects and toxicity: Many conventional antibiotics have associated side effects and can be toxic to the body, especially when used for prolonged periods.
Natural treatments, such as chlorine dioxide, may offer a lower toxicity profile and reduced side effects. This is particularly beneficial for vulnerable populations, such as children, pregnant women and the elderly, who may be more susceptible to the side effects of conventional antibiotics.
7. Preservation of the intestinal microbiota: Conventional antibiotics often disrupt the balance of beneficial bacteria in the gut, leading to dysbiosis and potential long-term health consequences.
New and natural therapies can offer targeted approaches that selectively eliminate harmful bacteria while maintaining the diversity and function of the gut microbiota.
This maintenance is vital as a healthy gut microbiome plays a vital role in immune function, digestion and overall wellbeing.
8. Sustainable and environmentally friendly solutions: The production and use of conventional antibiotics can have adverse environmental impacts, including the development of antibiotic-resistant strains in the environment.
Natural remedies often come from renewable sources, such as plants or compounds derived from microbes, which can be produced in a sustainable way. In addition, these treatments can have minimal environmental impact as they often break down more easily, reducing the risk of long-term ecological damage.
9. Possibility of combination treatments: Natural therapies can be combined with conventional antibiotics or other alternative treatments to create synergistic effects and improve therapeutic outcomes.
This approach allows for personalised and tailored treatment regimens, optimising the potential benefits of each treatment method.
Combination therapies may be more effective in fighting resistant bacteria, reducing treatment time and preventing further development of resistance.
10. Accessible and affordable treatment options: Access to conventional antibiotics may be limited or cost-prohibitive in many parts of the world.
Natural treatments derived from locally available sources may offer more accessible and affordable options for treating resistant infections.
This can have a significant impact on global health, particularly in resource-limited settings where the burden of antibiotic resistance is high.
In the search for effective alternatives, chlorine dioxide has emerged as a promising solution for the elimination of antibiotic-resistant bacteria.
It works by disrupting the cellular structures of bacteria, preventing them from multiplying and causing further damage.
Advantages of chlorine dioxide
Chlorine dioxide has emerged as a promising weapon in the fight against these resistant pathogens.
Its broad-spectrum activity, residual efficacy, reduced probability of resistance and environmental safety make it an invaluable tool for the elimination of antibiotic-resistant bacteria.
By embracing chlorine dioxide as part of comprehensive infection control strategies, we can significantly reduce the mortality rates associated with these infections, safeguard public health and address the growing problem of antibiotic resistance.
There are many advantages to using chlorine dioxide to treat antibiotic-resistant microorganisms, such as Spectrum activity:Chlorine dioxide has demonstrated efficacy against many bacteria, including MRSA and other antibiotic-resistant strains.
Its ability to target the bacterial cell wall and disrupt key metabolic processes sets it apart as an effective antimicrobial agent.
Residual effectiveness: Unlike traditional disinfectants, chlorine dioxide exhibits residual activity, which protects surfaces even after initial application.
This residual action is vital in healthcare settings where surfaces can become contaminated quickly, providing a persistent defence against bacterial colonisation and transmission.
Reduced likelihood of developing resistance:
The mechanism of action of chlorine dioxide reduces the likelihood of bacteria developing resistance.
Unlike traditional antibiotics that target specific bacterial components, chlorine dioxide attacks multiple cellular structures simultaneously, making it more difficult for bacteria to develop resistance mechanisms.
Elimination of biofilms: research studies have shown that chlorine dioxide penetrates and eliminates biofilms.
Biofilms are estimated to be 1000 times more resistant to antibiotics than free cells.
Environmental safety:
Chlorine dioxide is recognised for its favourable ecological profile. It decomposes into harmless by-products, leaving no toxic residues.
This feature ensures that its use for disinfection purposes does not contribute to long-term environmental damage.
The potential impact:
The importance of chlorine dioxide in the elimination of antibiotic-resistant bacteria cannot be overstated.
By providing an alternative treatment option, chlorine dioxide can help combat the growing problem of antibiotic resistance, reduce mortality rates and ease the burden on healthcare systems.
Its effectiveness against MRSA and other resistant strains can improve patient outcomes, reduce hospital stays and lower healthcare costs.
Cost - effectiveness:
Chlorine dioxide solution is cheap and can significantly reduce a country's healthcare costs over time.
Conclusions
This research focused on studying the effectiveness of chlorine dioxide in vitro for some of the most critical antibiotic-resistant bacteria that cause millions of deaths annually on a global basis.
We demonstrated that the optimal concentration of chlorine dioxide leading to almost complete disinfection in vitro is 7 ppm (ppm (p<0.01).
This is a safe dosage to take, as it is approximately the dosage used for water treatment.
What has been observed in vitro will probably also be observed in the human body.
Like blood, chlorine dioxide releases oxygen when it encounters acidity, either from lactic acid or from the acidity of the microorganism.
When chlorine dioxide breaks down, it releases oxygen into the blood, as do red blood cells (RBCs), through the same principle (known as the Bohr effect), which is to be selective for acidity.
Chlorine dioxide is a size-selective antimicrobial agent that can rapidly kill micron-sized organisms, but cannot cause real harm to much larger organisms, such as animals or humans, as it cannot penetrate deep into their living tissues.
There has been much controversy surrounding the use of chlorine dioxide.
However, it should be borne in mind that, as with any drug or supplement, the effects of exposure to any substance depend on the route of administration (e.g. inhaled, topical or oral), the state of the molecule (e.g. gaseous or aqueous), the concentration of the dose, the duration of exposure, personal characteristics and habits, and whether other chemicals or impurities are present.
Stressing that many toxicological studies have been carried out over the years with chlorine dioxide in humans and animals, showing its safety and efficacy, as it has been used in many applications to ensure that humans are exposed at safe levels.
When used properly at the low doses required to neutralise microbes' chlorine dioxide has been shown to be safe.
There were positive results in recent chlorine dioxide clinical trials conducted for COVID-19 by Insignares - Carrione in 2021, where highly pure chlorine dioxide CDS (2,990 ppm) was administered intravenously to patients.
In addition, government approvals of chlorine dioxide solutions for the prevention and treatment of the COVID-19 pandemic in Bolivia became law in 2020.
By which an ethics committee was legally established and approved by the Bolivian Ministry of Health, which, through its clinical, scientific and ethical research committees, conducts its research on chlorine dioxide for use in various applications.
Further, extensive clinical applications of chlorine dioxide in Epstein-Barr virus (EBV), cytomegalovirus (CMV), hepatitis A, B virus, HIV (AIDS virus) and others are constantly being used.
Further research is investigating the clinical use of chlorine dioxide, including non-specific spores, bacteria and viruses over the years.
There are hundreds more testimonials about the use of chlorine dioxide from volunteers collected over the years by the Jim Humble για διάφορες εφαρμογές του διοξειδίου του χλωρίου.
Clinical trials should be carried out to gain clinical experience of what would work best in clinical practice.
Clinicians using intravenous infusions may use 5 ml ampoules of CDSpure (2,990 ppm) directly or orally when diluted to the required levels.
Conflict of interest: None
Funding Statement: None
Η πρωτότυπη μορφή της έρευνας στο Scribd.
Eradication of Antibiotic Resistant Bacteria Using Chlorine Dioxide.
Eradication of Antibiotic Resistant Bacteria Using Chlorine Dioxide by sfagi on Scribd
Δημοσιεύθηκε: 2023
Παραπομπή: Γεωργίου Γ, Kotzé A, et al., 2023. Eradication of Antibiotic-Resistant E. coli, S. aureus, K. pneumoniae, S. pneumoniae, A. baumannii, and P. aeruginosa with Chlorine Dioxide In Vitro, Medical Research Archives, [online] 11(6).
https://doi.org/10.18103/mra.v11i7.2.4218
Copyright: © 2023 European Medical Association. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use,
distribution and reproduction in any medium, provided that the original author and source are acknowledged.
DOI
https://doi.org/10.18103/mra.v11i7.2.4218
ISSN: 2375-1924
RESEARCH ARTICLE
Elimination of antibiotic-resistant E. coli, S. aureus, K. pneumoniae, S. pneumoniae, A. baumannii and P. aeruginosa by chlorine dioxide in vitro
George Georgiou - Principal Investigator - admin@docgeorge.com
Agnieszka Kotzé - Researcher - aggie.kotze@gmail.com
Published: June 30, 2023
Citation: Georgiou G, Kotzé A, et al., 2023. Eradication of Antibiotic-Resistant E. coli, S. aureus, K. pneumoniae, S. pneumoniae, A. baumannii, and P. aeruginosa with Chlorine Dioxide In Vitro, Medical Research Archives, [online] 11(6).
https://doi.org/10.18103/mra.v11i7.2.4218
Copyright: © 2023 European Society of Medicine. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use,
distribution, and reproduction in any medium, provided the original author and source are credited.
DOI
https://doi.org/10.18103/mra.v11i7.2.4218
ISSN: 2375-1924
RESEARCH ARTICLE
Eradication of Antibiotic-Resistant E. coli, S. aureus, K. pneumoniae, S. pneumoniae, A. baumannii, and P. aeruginosa with Chlorine Dioxide In Vitro
George Georgiou – Principal Investigator – admin@docgeorge.com
Agnieszka Kotzé – Researcher – aggie.kotze@gmail.com